A Week In The Life” is a weekly Zikoko series that explores the working-class struggles of Nigerians. It captures the very spirit of what it means to hustle in Nigeria and puts you in the shoes of the subject for a week.
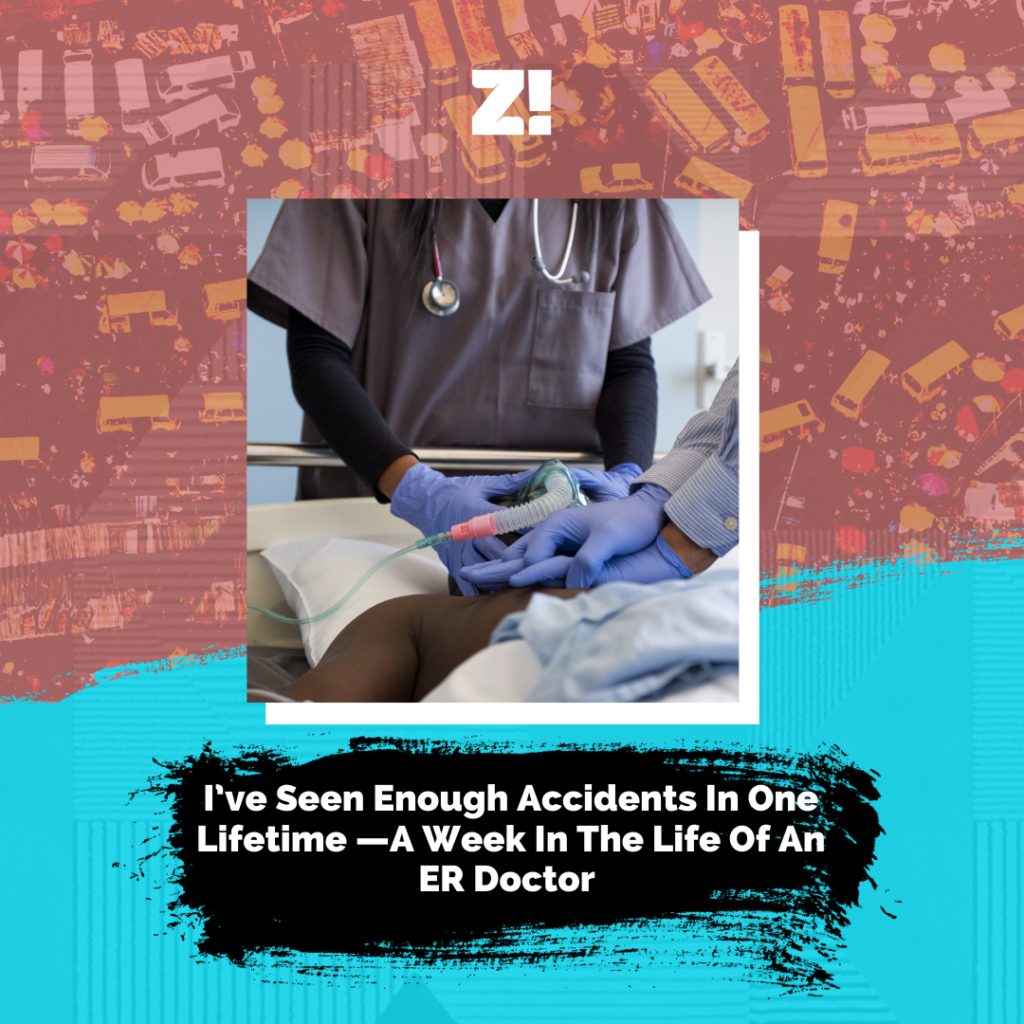
The subject of today’s “A Week In The Life” is an emergency room doctor at the Lagos State Accident and Emergency Center. He talks to us about the stress that comes with his job, how witnessing road accidents has made him more cautious, and the procedure for contacting emergency services in Lagos.
MONDAY:
Because everyone is rushing to beat Lagos traffic, Mondays are one of the busiest days for me. And I’m not saying this because I’m also stuck in traffic.
I start my day at 6 a.m. on most days. My routine is the same: I wake up for morning prayers, have my bath and freshen up, then I dress up.
Work resumes at 8 a.m. so I leave my house at 7 a.m. Because I work in an emergency centre, the first thing I do when I get to work is change into scrubs — a protective garment worn by healthcare professionals involved in patient care.
After that, I go to the emergency room to take over from my colleagues on the night shift. My colleagues hand over by briefing me on the history of patients on admission and treatments done so far. Somewhere between all the paperwork and catching up, my day fully starts.
On Monday, we get a lot of road traffic accidents and a high number of assault cases. Unsuspecting workers who leave their houses early to beat the traffic are sometimes attacked by hoodlums. Also, private cars and bus drivers who drive too fast in the early morning get into accidents.
My job involves resuscitating these patients and stabilising them. That is, keeping them alive long enough until they can get to a General hospital or to a specialist.
My first patient today stood out to me because he was a victim of assault. He was rushed in with a fractured skull and he had lost a lot of blood. I noted to the ambulance driver that I could only stabilise the bleeding, and he had to take the patient to LASUTH for specialist care.
After that patient, the rest of my day was a blur: stabilise this patient, repeat, stabilise that patient, repeat. Over and over again.
TUESDAY:
We get a lot of emergency cases every day and our response time is of utmost importance. When a patient enters our gate, the security personnel rings an alarm system to alert every healthcare worker in the facility to start running to the ER. You leave whatever you’re doing and run.
It takes less than two minutes to get to a patient, then treatment commences.
Before any contact with the patient, we put on our PPEs, gloves, disposable aprons, face mask and shields. Then we move to what we call initial patient evaluation and resuscitation. This follows a stepwise pattern known as A — E:
A — airway and cervical spine — spinal cord — protection
B — breathing & ventilation
C — circulation
D — disability or neurological deficit observation
E — environmental checks. You check the surroundings to eliminate any other form of injury that might have happened due to the environment.
Different doctors handle different parts of the protocol.
A: There’s a doctor whose job is to ensure that the airway is not compromised and the patient can breathe well. In addition, they also protect the cervical spine which houses the spinal cord. Protecting the spine is important because the lifting of a patient for treatment, especially after an accident, can damage important nerves connected to the diaphragm. And this can affect the supply of oxygen to the brain and heart, which can lead to death.
There’s another doctor in charge of monitoring the patient’s breathing. They ensure the patient has no injuries that can affect breathing. Then circulation where the doctor replaces body fluid of patients who are in shock due to reasons like bleeding or infection.
Finally, we check for disability and monitor the patient’s surroundings to ensure that we don’t miss anything. While all this is ongoing, the patient’s vitals like pulse rate, heart rate and oxygen level are being measured by the nurses.
Once the health team is satisfied with the patient’s stability, we then refer them for specialist management. A nurse accompanies the patient in our ambulance and hands over the patient to the new team that’ll resume management.
The best part? We do all this for free so that patients don’t have to worry about money. In an emergency, people just need to dial 121 and our ambulance will pick them up. Then our facility handles the rest.
WEDNESDAY:
Today, I’m thinking of how quickly things in the ER move from 0-100. One second you’re in your call room chilling and the next you hear the alarm ringing. And you start to run.
It can be overwhelming and demanding because you’re always on your toes. I remember being nervous on my first day of work because of the number of patients and the pace of the job. But now? I can function in my sleep.
It’s been a year since I started this job and the experience has given me self confidence. Now, I don’t panic and I never freeze.
I’ve also changed a lot since I resumed the job. I now take extra caution when driving by wearing my seat belt before leaving my house or office. I don’t drive more than 60km/h. And if I see a car speeding, I allow them to go past me.
When everyone is horning on the road, I put on my double-pointer [hazard light] and stay on one side of the lane. I let everyone overtake me because I’m not rushing anywhere.
I also don’t cross the express. If the pedestrian bridge is 30 minutes away, I’ll trek towards it and climb. I’ll also not be caught dead on a bike.
Why? I’ve seen enough road traffic accidents to last a lifetime. I know better.
We have a saying in the emergency centre: “What are you running for? Even if you go slow, you’ll still get to where you’re going.”
THURSDAY:
In this job, there’s no “off” switch that you can just turn off. The lines between home and work get blurred, especially for patients who have spent some time in the facility with us. I find myself constantly thinking about my patients even when I’m off work.
I’m happy that the Lagos state government pays the patient’s fees so we can focus on saving lives. In my experience, the delay from payment and deposit affects a patient’s chances of survival. But this way, we commence treatment quickly.
I wish there were more centres like this around the country. I also wish the health system as a whole was something to be proud of. If things worked well and doctors had equipment, maybe jaapa would reduce. I love my job, but I know it’s a bubble so I’m still making plans to leave for greener pastures.
The experience has opened my eyes to many possibilities. When I get abroad, I know that I’d like to still continue as an emergency responder. The adrenaline and fulfilment from helping patients is second to none.
But away from daydreaming to the present. We have a lot of accident cases today. But I’m not worried —with our level of care and protocols, we’re fortunate to have a low mortality rate. For that, Glory be to God.
I can’t wait to close from work in the evening and crash on my bed. I’m on the night shift tomorrow, and I need all the rest I can get. Fridays are also one of the busiest days because of TGIF accidents. But until I have to think of Friday, my plan is simple: I must survive today’s madness.
Check back every Tuesday by 9 am for more “A Week In The Life ” goodness, and if you would like to be featured or you know anyone who fits the profile, fill this form.
COMPONENT NOT FOUND: donation